Researchers have made a major breakthrough in the fight against drug-resistant tuberculosis (TB) in children by developing new, better-tasting treatment options. This advancement comes as global health experts raise concern over the 25,000 to 32,000 annual cases of rifampicin or multidrug-resistant TB (RR/MDR-TB) reported in children under 15.
The development was part of the ChilPref ML study, led by Stellenbosch University in South Africa and supported by the TB Alliance with funding from Unitaid. The study focused on making moxifloxacin—a key component of TB treatment—more palatable for children.
Dr. Anthony Garcia-Prats, a co-author of the study and associate professor at the University of Wisconsin-Madison, said the effort represents a shift in how treatment for pediatric TB is approached.
“We’re finally prioritizing children’s needs—starting with something as basic as making medicine taste better,” he said.
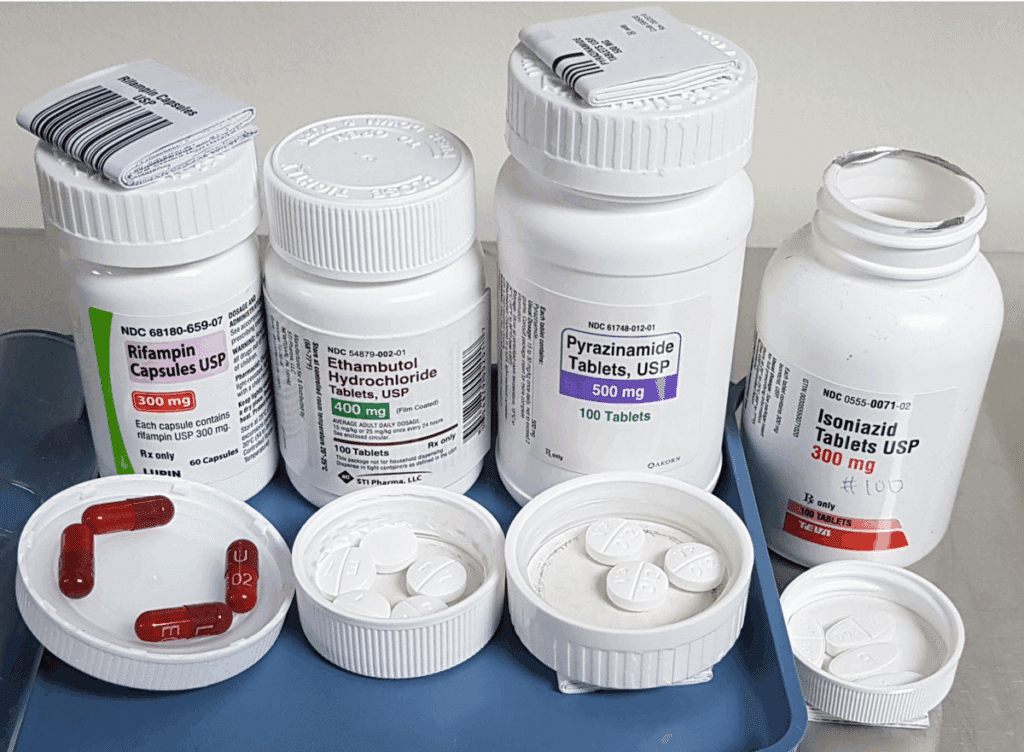
Moxifloxacin is one of the four drugs in the BPaLM regimen used for treating resistant TB strains. While not yet recommended for very young children as part of the full BPaLM combination, moxifloxacin is still often used in pediatric regimens. This makes its taste and ease of administration critically important.
Lead investigator Graeme Hoddinott emphasized that treatment can last up to nine months—an extremely long period for parents to struggle daily with administering bitter-tasting drugs to young children.
“We can’t expect humane treatment for kids when they’re being forced to swallow something they find repulsive every day,” Hoddinott said.
The study found two improved versions of moxifloxacin significantly more tolerable than generic options, offering hope for improved adherence and outcomes. The team also engaged children directly to understand their taste preferences—a step often overlooked in drug development.
Koteswara Rao Inabathina of the TB Alliance noted that the partnership with pharmaceutical manufacturers was key to creating these improved formulations.
“It’s not just about having effective medicines—it’s about making sure they’re actually usable by the patients who need them most,” he said.
The implications go beyond just moxifloxacin. The study showed that the process is safe, affordable, and can be used for other TB treatments and diseases, paving the way for more child-centered approaches in drug development.
Unitaid’s Cherise Scott echoed this, stressing that children’s needs should not be sidelined in global health efforts simply because they require more thoughtful approaches.
“Making treatment easier for children dramatically increases the chances of successful recovery,” Scott said.
This new step in TB care could significantly change outcomes for thousands of children worldwide who face a long and difficult road to recovery.




