Mpox formerly known as monkey pox, is a viral zoonotic disease caused by the monkey pox virus, which belongs to the same family of viruses as variola virus, the causative agent of smallpox. Although mpox is clinically less severe than smallpox, it can still lead to significant health issues, especially in vulnerable populations. This article provides a detailed yet concise overview of mpox, covering its history, transmission, symptoms, prevention, and treatment.
History and Background
Mpox was first identified in 1958 when outbreaks occurred in colonies of monkeys kept for research, hence the name “monkeypox.” However, the first human case was recorded in 1970 in the Democratic Republic of the Congo (DRC). Mpox cases have since been reported sporadically in Central and West African countries, particularly in regions close to tropical rainforests where the virus circulates among wild animals.The virus has two distinct genetic clades: the Central African (Congo Basin) clade, which tends to be more severe, and the West African clade, which is generally milder. The recent surge in cases outside Africa, particularly in non-endemic countries, has raised global health concerns, prompting the World Health Organization (WHO) to rename it “mpox” to reduce stigma and improve global response efforts.
Transmission
Mpox is primarily a zoonotic disease, meaning it is transmitted from animals to humans. The virus can spread through direct contact with infected animals such as rodents and primates, or by handling animal products like meat or skin. The exact animal reservoir is unknown, but it is believed that rodents, particularly African squirrels and rats, are major carriers of the virus.Human-to-human transmission occurs mainly through close contact with respiratory droplets, bodily fluids, or skin lesions of an infected person. It can also spread via contaminated materials like bedding or clothing. Unlike viruses that spread primarily through aerosols (like the flu), mpox generally requires prolonged face-to-face contact for transmission, making household members and healthcare workers more vulnerable.
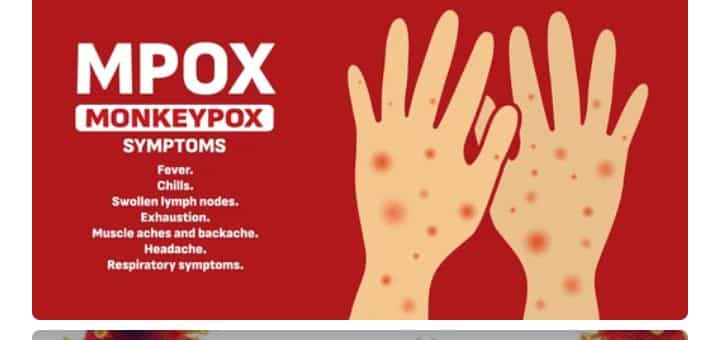
Symptoms
Mpox has an incubation period of 5 to 21 days. The disease typically begins with non-specific symptoms similar to other viral infections, including:- Fever- Headache- Muscle aches- Backache- Swollen lymph nodes- Chills- Exhaustion. A few days after the onset of fever, a rash develops, starting on the face before spreading to other parts of the body, particularly the palms and soles. The rash progresses through several stages, including macules, papules, vesicles, pustules, and finally, scabs. This rash is one of the most characteristic features of mpox and can last for two to four weeks. In severe cases, the lesions can be painful, leading to complications such as secondary infections, bronchopneumonia, sepsis, encephalitis, or eye infections that may result in loss of vision.
Diagnosis
Given its similarity to other rash-causing illnesses such as chickenpox, measles, and smallpox, accurate diagnosis is essential. Laboratory confirmation is typically done using polymerase chain reaction (PCR) tests, which detect viral DNA from lesion samples. The identification of the virus is crucial for distinguishing mpox from other diseases with similar clinical presentations.

Prevention
Preventing mpox requires a multi-faceted approach. The primary method of prevention in endemic areas involves reducing the risk of zoonotic transmission. This includes avoiding contact with wild animals, particularly those that are sick or dead, and thoroughly cooking meat before consumption. People should also avoid contact with materials that may have come into contact with infected animals. For human-to-human transmission, key preventive measures include isolating infected individuals, wearing personal protective equipment (PPE) for healthcare workers, and practicing good hand hygiene.
The smallpox vaccine, which provides cross-protection against mpox due to the genetic similarities between the two viruses, has been shown to be about 85% effective in preventing mpox. While routine smallpox vaccination was discontinued after the disease was eradicated in 1980, newer vaccines like JYNNEOS (also known as Imvamune or Imvanex) have been developed for use in populations at risk of mpox infection.
Treatment
Currently, there is no specific treatment for mpox. Most cases are mild and self-limiting, with patients recovering within 2 to 4 weeks. Treatment is mainly supportive, focusing on relieving symptoms and preventing complications. For severe cases, antiviral medications like tecovirimat (TPOXX), initially developed for smallpox, have been used under emergency protocols. In addition to antivirals, post-exposure prophylaxis (PEP) using the smallpox vaccine may help prevent infection if administered within four days of exposure. Vaccination can reduce the severity of illness even if given later, though effectiveness diminishes after four days.
Global Impacts and Future Challenges.
The global outbreak of mpox in 2022, with cases reported across Europe, the Americas, and parts of Asia, underscored the importance of preparedness and rapid response to zoonotic diseases. Many of the cases in these outbreaks were linked to international travel or close human contact in social networks. The rapid spread in non-endemic countries raised questions about the potential for mpox to become a more widespread health threat. While most cases in these outbreaks have been mild, vulnerable groups, including immunocompromised individuals, young children, and pregnant women, remain at higher risk of severe disease. Public health authorities have since emphasized the importance of monitoring, timely vaccination, and public awareness campaigns to prevent further spread.
Mpox, while not as deadly or contagious as smallpox, represents a growing public health concern, particularly in an increasingly interconnected world. Effective surveillance, prompt isolation of cases, and vaccination strategies will be crucial in controlling future outbreaks. As the world continues to confront emerging and re-emerging zoonotic diseases, understanding the dynamics of mpox and implementing robust prevention measures will be critical in mitigating its impact on global health.




